The healthcare industry is one of the most highly regulated industries in the world. This is to be expected, considering public health and safety depend on it. As such, companies in the healthcare industry must track a variety of data about their operating conditions to validate compliance with those regulations.
A variety of data loggers get enlisted to record that data, but temperature data loggers carry special importance in the healthcare industry. Temperature matters at nearly every stage of the industry. In healthcare, the doors don’t stay open and the lights don’t stay on unless temperature data loggers do their job.
A Quick Primer on Data Loggers
Digital data loggers are automated devices that record, at set intervals, data from the surrounding environment.
The device itself contains three core components — a sensor, a microprocessor, and a storage drive.
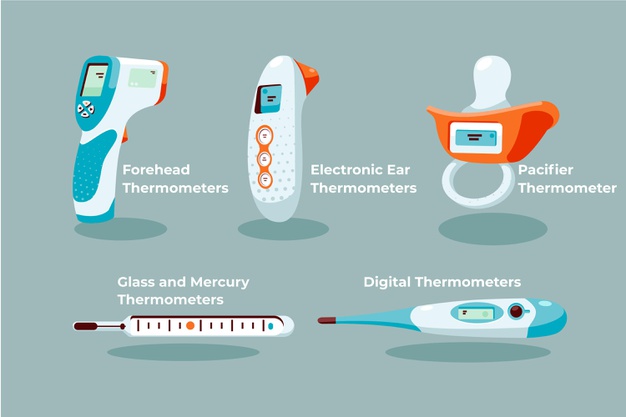
The sensor detects the surrounding conditions. Data logger sensors might detect ambient temperature, pressure, voltage, or any other condition that must be monitored. Temperature data loggers use thermometer sensors, but the sensors may vary in sensitivity to handle extreme heat or extreme cold.
The signal from the sensor is interpreted by the microprocessor and translated into digital data, which then gets recorded on the storage drive.
Once the data has been recorded, it can be retrieved from the storage drive in a variety of manners. The device may offer USB data transfer to other devices, or it may have WiFi/IoT capability to upload the data directly to the Cloud. Sophisticated data loggers pair with validation software to automatically compile regulator-approved charts.
Dickson has a few examples of temperature data loggers that are often used in healthcare and related fields.
Four ways temperature data loggers are used in healthcare.
1. Vaccine Monitoring
As of this writing, the world is in the midst of the largest vaccine manufacturing campaign in human history. Faced with the deadly COVID-19 pandemic, pharmaceutical industries rushed to create a safe and effective vaccine against the novel coronavirus.
Many succeeded in record time and in defiance of all expectations, with two vaccines achieving emergency use authorization by the FDA less than a year after the SARS-CoV-2 genome was made public.
When the vaccines made their debut, one of the best-known facts about them was that they had to be stored at extremely cold temperatures, presenting a logistical challenge. The Pfizer/BioNTech vaccine, the first to achieve emergency use authorization, has particularly stringent temperature requirements. It must be kept at minus-70 degrees Celsius — colder than the average temperature of Antarctica. Transporting it long distances, and then keeping it in small facilities with limited resources to acquire deep freezers, presented a logistical hurdle to distribution.
Vaccine temperature requirements must be adhered to carefully. Otherwise, the vaccine can lose its potency. The World Health Organization (WHO) recommends that vaccines be stored with temperature data loggers in the storage unit, as close to the vaccines as possible, and that temperature be continually monitored and recorded at least once a day.
In the case of a substance like the Pfizer/BioNTech COVID-19 vaccine, the temperature data logger must be sensitive and durable enough to handle the temperatures of deep freeze required to maintain the vaccine’s potency.
Temperature-sensitive products like vaccines must be transported in a cold chain, with temperature verified at every stage of the transport and storage process — factory, refrigerated truck, warehouse, and so on. Temperature data loggers are used to verify the cold chain at every stage.
2. Medical Device Manufacturing
Doctors and other healthcare professionals depend on reliable medical devices to monitor patient conditions, diagnose illness, and perform complex procedures like surgery.
Medical devices get rated in three classes, from the relatively low-risk Class I to the life-sustaining Class III. In the case of Class II and Class III medical devices, a manufacturing flaw could mean a life-or-death difference in the survival of a patient in serious or critical condition.
Because of this, medical device manufacturers operate under some of the most strict regulations of any manufacturers. To maintain their FDA registration, medical device manufacturers must religiously monitor multiple temperatures within their facilities.
This includes the temperatures at which the components and finished devices are stored to prevent warping and corrosion, as well as keeping them sterile. It also includes the high temperatures in furnaces to ensure proper annealing and tempering without unexpected or unnecessary expansion.
Due to the extreme temperature variance in manufacturing processes, data loggers of different sensitivities and resolutions must be used throughout the facilities to maintain all necessary compliance records.
3. Chamber Monitoring
A chamber is any controlled space, and the healthcare industry needs a lot of them. A chamber could be a room in which a patient in a fragile condition is placed to recover. It could also be a laboratory in which a critical drug or treatment is tested. Without control of the chamber, you can’t produce repeatable results, because the conditions of the procedure have changed.
In addition to producing repeatable, reliable results, healthcare chambers may be subject to regulatory audits. Temperature data loggers, as well as humidity and other data loggers, are routinely relied upon to produce audit-ready reports of chamber conditions so that they can pass inspection and remain in operation.
4. Pharmaceutical Production
The medical device manufacturing industry may be heavily regulated, but the pharmaceutical industry could go toe-to-toe with them in terms of regulatory burden. That’s to be expected — people ingest pharmaceutical products and depend on them for their health and wellbeing. In some cases, they depend on pharmaceuticals for their very survival. There’s no room for error.
Pharmaceutical companies like Pfizer and Moderna formulated, tested, and produced the above-mentioned COVID-19 vaccines, which are very sensitive to temperature. Moreover, those vaccines could not have been created without compliant laboratory and manufacturing facilities, which must be kept within strict temperature ranges to ensure the quality of the product output.
Finally, temperature-sensitive medications have their own cold-chain requirements. Storage temperatures must be carefully monitored from the factory to the transport container to the warehouse to the retail shelf and beyond. At each point in this cold chain, you will find temperature data loggers and probably more than one.
Temperature data loggers are the unsung heroes of the healthcare industry, working quietly and thanklessly in the background to ensure that we enjoy effective and high-quality healthcare products and services. Not bad for a sensor, a microprocessor, and a storage drive.